Setting Quality Metrics for Value-Based Pay - Part One
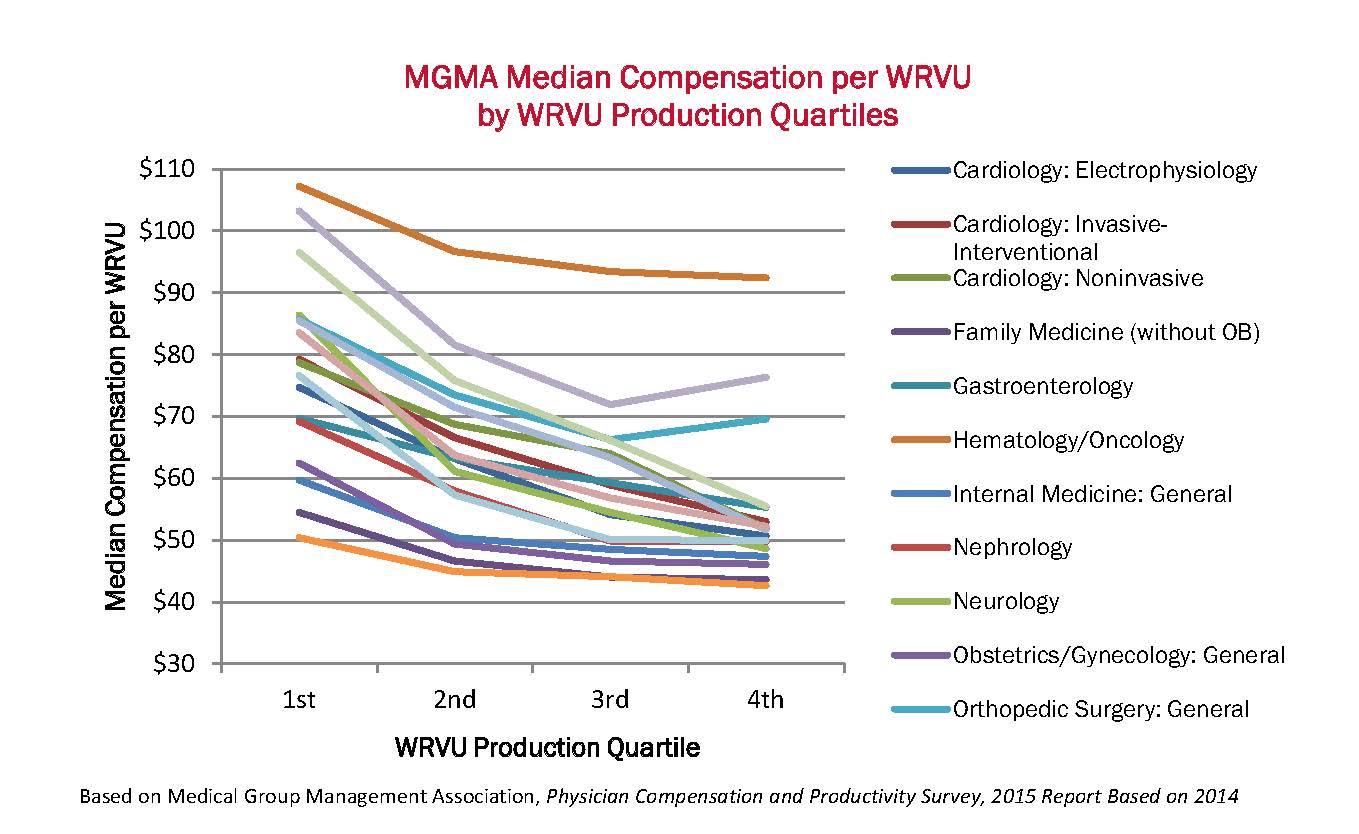
Government and commercial insurers are transforming payment models from fee-for-service (FFS) to arrangements that include incentives for quality, outcomes, improved patient satisfaction, and reduced cost. In the FFS environment, hospitals, physicians, and other providers have been subjected to insignificant financial risk relative to the risk borne by payers; however, with time, transformed payment arrangements have encouraged, if not required, more providers to assume downside risk. Why? One reason is to hold providers accountable for the cost and quality of care. The table below by The Commonwealth Fund summarizes this need by showing where the United States ranks relative to other industrialized nations in health outcomes and risk factors:
Continue reading >