My Hospital is Losing Millions on Physician Practices—Part Two
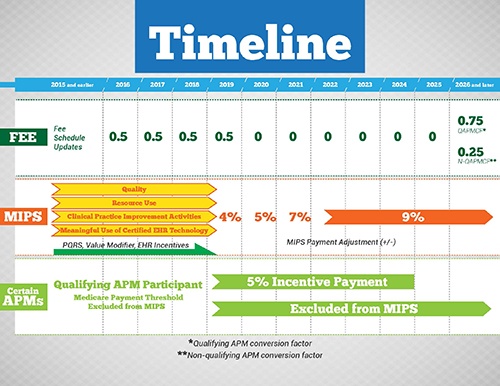
We described in the previous installment in this series how recent case law and DOJ settlements provide clear evidence of the position of qui tam relators, prosecutors, and government experts that losses on hospital operation of physician practices are being targeted. Because evidence suggests that hospital losses on physician practices are common in many markets, the questions on everyone’s mind are whether health system losses on physician practices put the organization and key individuals at significant fraud and abuse compliance risk, to what degree can existing physician practice losses be justified through documentation, whether the health system has a functional Fair Market Value (FMV) and Commercial Reasonableness (CR) enterprise risk management process, and—the subject of this series--is a plan at the ready to begin mitigating practice losses?
Continue reading >