A Bridge for Healthcare Reform
Over the past decade, clinical co-management arrangements (CCMAs) have risen in popularity as a means to achieve a more integrated care delivery model. CCMAs have often been touted as an interim strategy to bridge hospitals to newer emerging models, but many hospitals have yet to cross that bridge.
The primary benefit of most CCMAs is the creation of a contractual structure to help achieve several goals:
- Elevate physician leadership to assist in the oversight of a particular service line;
- Align physicians and hospitals with a focus on quality and process improvement; and
- Reward physicians for cost reductions, quality performance, and time invested.
CCMA payments to the physicians are set in advance. They include base management fees for time spent providing administrative services and incentive compensation to reward pre-determined program goals. Hospitals often redirect call coverage and medical director payments to the CCMA to help support the value paid under the arrangement; however, determining a CCMA’s overall financial return for a hospital is a bit more nuanced.
The most successful CCMAs support hospital goals through meaningful data analytics that allow engaged physician leaders to track quality and cost performance. But in many cases, cost savings and other financial benefits generated under the CCMA (excluding referrals of designated health services) are not well documented. To add further complications, studies have shown that not all improvements in quality are correlated to reductions in cost.
Under poorly designed arrangements, hospitals may pay physician management fees while simultaneously receiving payment reductions under Medicare’s value-based payment program or incurring increased costs due to a mismatch in goals and payment structures. Such a misalignment raises questions related to the Stark Law’s commercial reasonableness requirements. Particularly, poor performing hospitals should ask if the arrangement is “a sensible, prudent business agreement, from the perspective of the particular parties involved, even in the absence of any potential referrals.”[1] As such, hospitals with poor performing CCMAs should ask themselves whether their lack of financial return is also creating compliance risk and if the CCMA is still the best alignment option.
MACRA Paves the Way for New Models
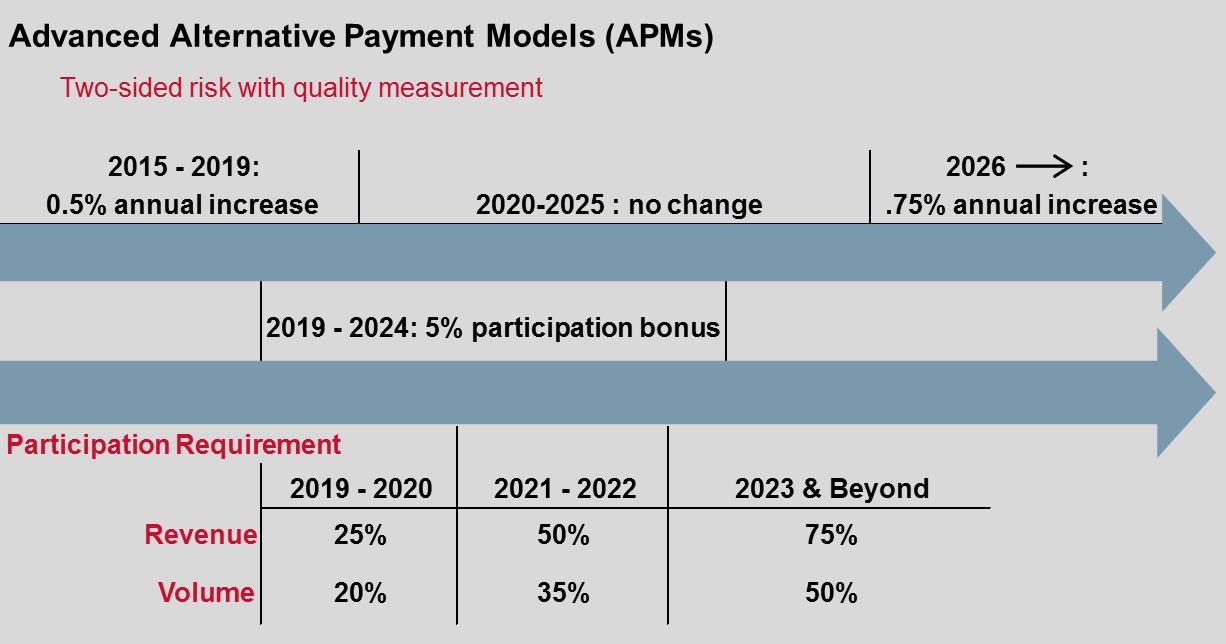
For hospitals with successful CCMAs and the proper infrastructure, now may be the time to consider crossing the alignment bridge and transitioning to a shared savings program under an advanced alternative payment model (APM). Under MACRA, physicians are encouraged to participate in advanced APMs (such as MSSP Track 1+, Track 2, and Track 3) through several financial incentives:
- 5% participation bonus applied to Medicare revenues from 2019 to 2025,
- .75% annual increase in Medicare base fees after 2026, and
- Potential for a material financial upside annually for high-performing physicians.
 For more information about APMs and MACRA, click here
For more information about APMs and MACRA, click here
Advanced APMs require that physician payments are based on quality measures and that physicians share in “more than nominal financial risk for monetary losses.” Similar to CCMAs, advanced APMs elevate physician leadership and align hospital and physician incentives while tying performance to quality and cost improvements. Advanced APMs also provide several advantages over CCMAs:
- Payments to physicians are based on documented additional revenue streams based on shared savings.
- MACRA payment incentives for physicians help to subsidize the financial return for physician efforts and invested time.
- Shared savings can be passed on to physicians through CMS/OIG waivers if specified conditions are met,[2] allowing for stronger regulatory compliance.
Alignment Transition
For hospitals that lack the IT infrastructure or quality performance, and for hospitals in markets without shared savings options, CCMAs may still serve as the needed bridge to future alignment strategies. If so, these hospitals should take necessary steps to improve cost measurement and incorporate elements of emerging reform models into their existing CCMAs, where applicable.
For hospitals that have achieved success under the CCMA model, now may be the time to start your transition to a new alignment strategy. Wherever you are in the process, we advise hospitals to engage healthcare legal counsel and consultants with the experience to help navigate key regulatory and financial considerations.
For weekly insights into healthcare, please sign up here:
[1] 63 Fed Reg 1700 (Jan. 9, 1998).
[2] 80 Fed Reg. 66726 (Oct. 29, 2015).




Leave A Comment