Charles Darwin might have been talking about the world of healthcare when he said, “It is not the strongest of the species that survives, nor the most intelligent, but the one most responsive to change.”

Amazon is famously adept at responding to change. This disruptor of industries is collaborating with leaders in finance (JP Morgan Chase) and investment (Berkshire Hathaway) to solve the problem of rising healthcare costs. These three powerhouses have the money, power and talent to truly move the needle toward the Triple Aim of better care, smarter spending and healthier people.
For decades, that goal has remained challenging for legacy healthcare organizations. The industry has made progress on a number of fronts, but providing quality care in a cost-efficient manner remains an elusive goal for a number of reasons. Some of the challenges that we see plaguing our clients are:
1. Payment model reform continues to move forward—but in fits and starts.
Healthcare providers still have a foot in two boats. For most, the majority of revenue still comes from fee-for-service contracts. MACRA was intended to force forward momentum, but with Congress and CMS tapping the brakes on MIPS implementation, it is becoming easier for many providers to follow suit. (The announcement of the new bundled payments initiative offered some reassurance that HHS is still committed to moving providers into alternative payment models.).
2. Hospitals are struggling with margin pressure.
As hospitals search for ways to shore up erosion of inpatient revenue, they are looking to cost-cutting measures as well as diversification. What has become increasingly clear is that a focus on increasing inpatient volume will not be enough to counteract the continued margin compression. As a result, hospitals are turning their attention to less-costly outpatient settings, often partnering or integrating with providers such as urgent care and emergent care centers. Other strategies include improvements in revenue cycle systems and organizational restructuring to take advantage of efficiencies.
3. Physician incentives are not yet aligned with value-based payment goals.
Most doctors still are paid based on production. These “eat-what-you-kill” incentives fail to motivate the behavior change that is necessary for success under value-based payment programs.
4. Good cost and quality data remains elusive.
Data is essential to making the improvements in quality and cost-efficiency required to succeed in value-based payment models. Participation in one or more of the CMS bundles requires pulling clinical, financial and claims data from many different places. Many physician practices and smaller hospitals lack the infrastructure to aggregate and analyze this data.
Opportunities for Healthcare Providers
These are significant headwinds, and yet we believe that healthcare organizations that are dedicated to improving the quality and efficiency of care can move the needle. We see three areas that will become increasingly important:
Collaboration—We will never solve the conundrum of how to deliver the right care in the right setting for lower cost until all the players are working together to achieve that goal. Bundled payment program participants know that success requires collaboration and agreement on the proper care protocol for the entire episode of care. Rather than acting as lone wolves, physicians in these payment models must cede some of their decision-making authority. Success in value-based payment models is driven by strong leaders who rally clinicians around their vision of delivering high-quality, efficient patient care.
Engagement—Patient engagement is critical to improving care. And yet, it often seems that the system is designed to move the patient through as quickly as possible rather than to encourage patient questions. CMS chronic care management codes provide an avenue for providers to follow up with patients to make sure they are taking the important steps they need to get and stay healthy. However, they have limited effectiveness when the provider doesn’t control all the patient’s healthcare services. Technology will enable greater strides in engagement, and patient portals are just the beginning. Anticipate greater adoption by Millennials and Gen Z of technology solutions that make care more accessible, convenient and cost-effective.
Compensation—To succeed in value-based payment models, hospitals and physician practices must hold clinicians accountable for the right behaviors and performance. At the same time, those compensation models must attract and keep the best clinicians who are dedicated to value-based care. With the new opportunity from CMS to participate in a bundled payment initiative, we believe that 2018 is the year when physician compensation will start to truly transform.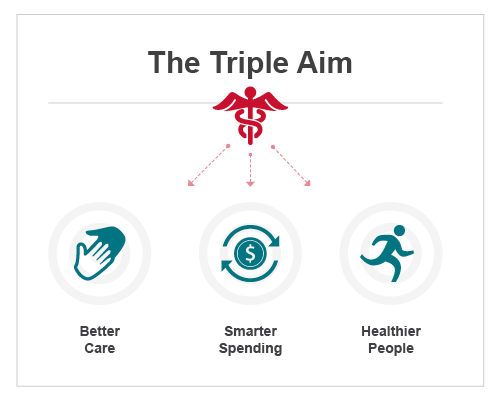
Healthcare organizations have much to learn from Amazon. This highly adaptive, consumer-centric company is willing to collaborate with organizations in completely different industries to solve one of the most pressing problems of our time. Take inspiration from this industry disruptor and seize opportunities in your own marketplace to collaborate with healthcare and non-healthcare companies in an effort to achieve the Triple Aim.
For weekly insights into healthcare, please sign up here:




Leave A Comment