The Bipartisan Budget Act of 2018 (BBA18), signed by President Trump on February 9, includes several provisions that will affect healthcare providers’ Medicare reimbursement—in both positive and negative ways.
In shades of the perennial override of the Sustainable Growth Rate adjustment (which MACRA was implemented to fix), Congress responded to provider concerns about the MIPS regulatory burden by extending the transitional period of the controversial payment track.
Healthcare providers who have been diligently working to meet the requirements of MIPS may be understandably frustrated by these delays; for many other participants who have struggled to make improvements, BBA18 provides much-needed relief.
Here, we examine the potential impact of some of these modifications mandated by BBA18.
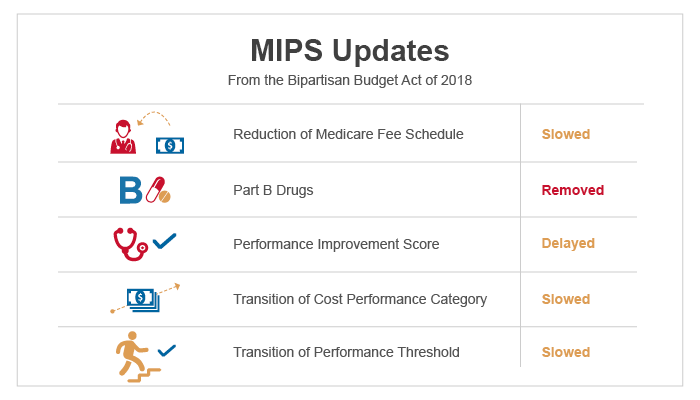

Reduction of Medicare Fee Schedule Update
Physicians will receive a smaller Medicare fee-for-service reimbursement increase in 2019 than originally planned. Rather than the 0.5 percent update to the Medicare Physician Fee Schedule (MPFS) that MACRA had established, BBA18 drops that to a 0.25 percent increase in 2019.
After 2019, MACRA suspends increases until 2026, when Qualified Participants in Alternative Advanced Payment Models (AAPMs) will receive an annual 0.75 percent increase and all other Eligible Clinicians will get a 0.25 percent increase.
These increases will likely fall far short of inflation, further underscoring the need for providers to develop strategies to move from MIPS into A-APMs.

Elimination of Part B Drugs from MIPS
Providers are commending Congress for eliminating the cost of Part B drugs from the calculation for the MIPS Cost performance category. The original wording in the Quality Payment Program (QPP) Final Rule for Calendar Year 2018 made clear that MIPS payment adjustments (both positive and negative) will be made for “items and services” under Medicare Part B, including Part B drugs. However, BBA18 has changed that wording to “covered professional services,” in effect eliminating Part B drugs from the payment adjustment for performance periods beginning in 2018.
MACRA’s critics welcome this change as a reversal of an unfair policy that penalized certain physicians, such as oncologists and rheumatologists, whose patients rely on expensive drugs.

Removal of Performance Improvement Score
The Improvement Activities category, which will measure improvement in the Quality and Cost performance categories, was supposed to go into effect for the 2018 performance year. However, Congress delayed the implementation of that category until 2022. This is disappointing news for providers that expect higher cost or quality scores in 2018. For participants that have struggled to make improvements, on the other hand, this provision provides an opportunity to gain some traction with value-based care processes before the new category goes into effect.

Slowing Transition of Cost Performance Category
Congress gave the Department of Health and Human Services (HHS) Secretary the flexibility to set the pace for the ramp-up of the Cost performance category weight. MACRA required that the Cost category represent no more than 10 percent of the Composite Performance Score in the first year of the program, up to 15 percent in the second year, and 30 percent in the third year. BBA18 softened that language, requiring only that the cost category represent not less than 10 percent and not more than 30 percent of the score in years two through five of the program.
Without legislative action, the Cost performance category will represent 30 percent of the Composite Performance Score in performance year 2022 (payment year 2024). While this provides some degree of relief to providers not yet fully adept at managing costs in the value-based environment, it does not completely eliminate costs from the equation.

Transition of Performance Threshold
The extended transitional period also allows the HHS Secretary to stretch out the ramp-up period for the MIPS performance threshold for three additional years. CMS had set the performance threshold at 3 points in the first year and 15 points in the second year. In 2019 and later years, it was originally planned to be set at a level where about half of clinicians would be above and half below the threshold. BBA18 authorized a more gradual transition from 2019 through 2021.
This is another effort by Congress to ease the burden on providers. A lower threshold essentially means more winners and fewer losers. The unfortunate downside for clinicians who have improved their cost and quality performance is that their positive payment adjustments will be smaller than they might otherwise have been. Since MIPS is a budget-neutral program, the positive payment adjustments must be counterbalanced by equal negative payment adjustments. This highlights our advice to many clients to have a strategy to move beyond MIPS to APMs and, ultimately, AAPMs as soon as feasible.
What You Can Do
Despite tapping the brakes, Congress has not repealed MIPS (yet). And given that federal regulators still appear committed to moving providers into alternative payment models, our advice continues to be that clinicians should be adopting changes that allow successful transitions to innovative and advanced care and payment models.
We recommend carefully studying the biannual Quality and Resource Use Report (QRUR), as well as other cost and quality data supplied by payers, to learn where your practice or health system stacks up relative to peers on quality and cost metrics.
Take advantage of this Congressional gift of an extended transitional period to continue to make patient care processes more team-based and patient-centric. Ultimately, those investments will reap the reward of positioning your practice or system for success—whether in MIPS or an APM.
We will remain abreast of developments in legislation and rulemaking around MACRA and other value-based payments. In the meantime, remember to submit 2017 MIPS data by March 31, 2018. This is the last date to avoid a negative payment adjustment or qualify for a positive payment adjustment in 2019.
For weekly insights into healthcare, please sign up here:




Leave A Comment